https://www.wahmg.com/)">
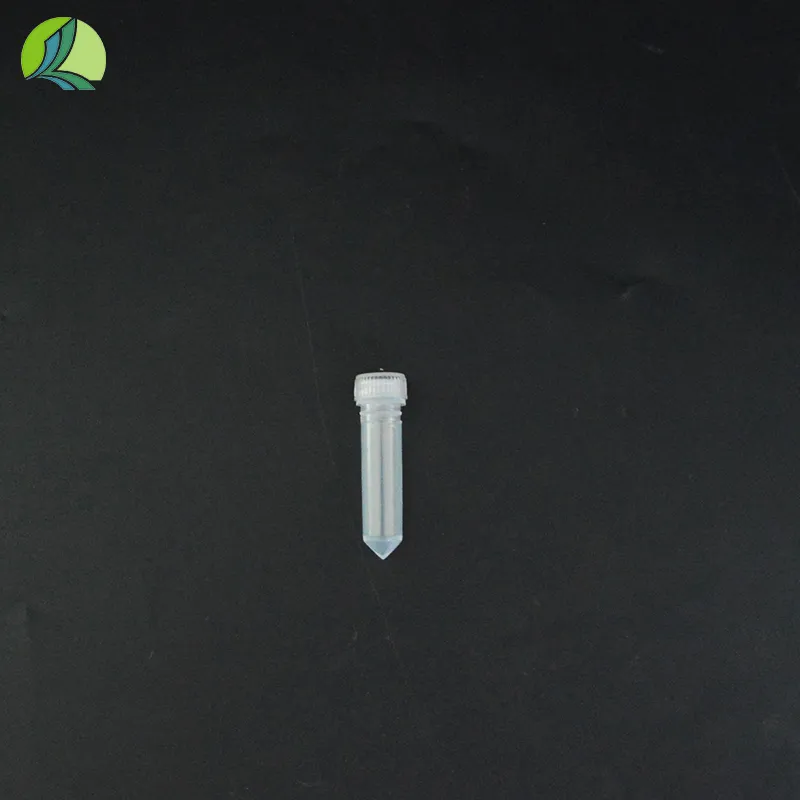
tube for plasma collection
tube for plasma collection
The Importance of Tubes for Plasma Collection in Medical Diagnostics
Plasma collection is a crucial procedure in the field of medical diagnostics and research, serving various purposes including blood tests, disease diagnosis, and therapeutic applications. To ensure the accuracy and reliability of test results, the use of appropriate tubes for plasma collection is essential. This article delves into the significance of these tubes, their design features, and best practices in plasma collection.
The Importance of Tubes for Plasma Collection in Medical Diagnostics
The effectiveness of plasma collection tubes is predominantly determined by their additives and material composition. Typically, these tubes are made from polyethylene or glass and often contain specific additives to facilitate clotting or prevent hemolysis. For plasma collection, anticoagulants such as EDTA, heparin, or citrate are commonly added to the tubes. These anticoagulants play a critical role in preventing the blood from clotting during and after collection, ensuring that a clear plasma sample can be obtained for further analysis.
tube for plasma collection

To optimize the plasma collection process, several factors must be considered. Firstly, it is essential to select the appropriate tube type based on the desired analysis. For instance, a tube containing EDTA is ideal for complete blood counts, while those with heparin are often used for biochemical tests. Secondly, the volume of blood collected must align with the tube's capacity, as underfilling or overfilling can jeopardize the test's accuracy.
Handling practices during plasma collection also significantly impact the final results. A thorough mixing of the blood sample with the anticoagulant is necessary to prevent coagulation. After collection, the tubes must be promptly inverted several times to ensure complete mixing. Neglecting this step may lead to sedimentation or clot formation, which can compromise the quality of the plasma sample.
Another key consideration in plasma collection is the proper storage and transportation of the collected samples. Plasma samples should be processed as soon as possible after collection. If immediate processing is not feasible, samples should be refrigerated at the appropriate temperature (usually between 2°C to 8°C) to preserve the integrity of the plasma for subsequent testing. Furthermore, plasma should be separated from the cellular components within a few hours of collection to minimize degradation of analytes.
In conclusion, the selection and use of appropriate tubes for plasma collection are pivotal in ensuring accurate and reliable test results in medical diagnostics. By understanding the various types of tubes, their additives, and the best practices surrounding plasma collection, healthcare professionals can enhance the quality of blood tests, ultimately leading to better patient care. With advancements in medical technology, ongoing research about plasma components will continue to evolve, emphasizing the need for high standards in plasma collection and analysis.
-
Wholesale Plastic Juice Bottles with Caps 16 oz Options Available Bulk Packaging SolutionsNewsJun.10,2025
-
Laboratory Apparatus Reagent Bottle – Durable & Chemical Resistant Bottles for Safe StorageNewsJun.10,2025
-
Squeezable Dropper Bottles Durable, Leak-Proof & CustomizableNewsMay.30,2025
-
Affordable Plastic Petri Plates Sterile & Disposable Lab-GradeNewsMay.30,2025
-
Eye Dropper Caps Precision 24/410 & Plastic Bottle-Compatible TipsNewsMay.30,2025
-
Affordable Mini Spray Bottle Price & Wholesale Deals Shop NowNewsMay.29,2025